What is arthritis?
Arthritis is a general term for inflammation of one or more of your joints. Pain, swelling, and stiffness are the primary symptoms of arthritis. Any joint in the body may be affected by the disease, but is most common in the knee and hip. Knee arthritis can make it hard to do many everyday activities, such as walking, climbing stairs, and often times results in night time pain as well. It is a major cause of lost work time and a serious disability for many people. The most common types of arthritis are osteoarthritis and rheumatoid arthritis, but there are several different forms. In 2012, more than 51 million people reported that they had been diagnosed with some form of arthritis, according to the National Health Interview Survey. While arthritis is mainly an adult disease, some forms affect children. Although there is no cure for arthritis, there are many treatment options available to help manage pain and keep patients active.
What causes osteoarthritis?
Osteoarthritis is the most common form of arthritis in the knee. It is a degenerative, "wear-and-tear" type of arthritis that occurs most often in people 50 years of age and older, but may occur in younger people too. Although there is a genetic component to osteoarthritis, years of wear and tear, prior surgery on your knee, or prior trauma to the knee increases your risk of osteoarthritis. In osteoarthritis, the smooth cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful bone spurs. Osteoarthritis develops slowly and the pain typically worsens over time. There are 3 main areas contained within the knee joint, medial, lateral and under the knee cap (patella). Arthritis can affect only one area or all 3 areas at once.
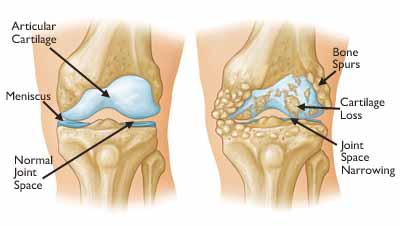
(Left) Normal joint space between the femur and the tibia. (Right) Decreased joint space due to damaged cartilage and bone spurs.
So you have arthritis of the knee. What are your options?
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and keep you active.
Nonsurgical Treatment
As with other arthritic conditions, the most appropriate initial treatment of arthritis of the knee is nonsurgical.
By far the most effective treatment to help with the pain and slow the progression of knee arthritis is maintaining a healthy weight. Being only 10lbs overweight increases the force on the knee by 30-60 pounds with each step!!!
Lifestyle modifications. Some changes in your daily life can protect your knee joint and slow the progress of arthritis.
-
Minimize activities that aggravate the condition, such as climbing stairs.
-
Switching from high impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling or elliptical) will put less stress on your knee.
-
Weight loss, weight loss, weight loss if the patient is overweight
An anti-inflammatory such as Meloxicam, Aleve, Ibuprofen, Advil, or Celebrex are great options to help with the pain and inflammation around the joint. I typically recommend one of these in our regimen if the patient tolerates NSAIDs. Remember all medications have side effects so check with your doctor before starting these.
“Corticosteroid” injections (aka cortisone shots): these are probably the most common tool we use to manage the pain and inflammation associated with arthritis. While the injections do not contain cortisone per se, they do contain a steroid, which is the strongest anti-inflammtaory available. I often get the question of “how long do these last?” or “Mr. X had 8 months of relief, but Mrs. Y only had 3 weeks relief…why?” The answer is everyone is different. Not every patient has the same degree of arthritis. Mr X may have mild OA while Mrs. Y may have “bone on bone arthritis”. As the arthritis progresses, we see the duration of relief get shorter and shorter. My suggestion would be continue injections as long as you get good relief from them. If they are no longer helping at least 3 -4 months, we need to switch gears with our treatment options. You can only receive 3 to 4 steroid injections per year within a joint or more damage can occur to the remaining cartilage.
What about the lubrication injection? When you hear about lubrication injections, we are referring to a visco-supplementation. Some refer to it as “Rooster Comb” injections. There are several forms available. The thing about these injections is they work for some and not for others. We usually recommend them for mild to moderate arthritis, and find it less effective for patients with bone on bone arthritis. These are extremely expensive so we have to clear it through insurance, which can be tough and sometimes even denied.
Glucosamine and chondroitin sulfate: These substances found naturally in joint cartilage, can be taken as dietary supplements. Although patient reports indicate that these supplements may relieve pain, there is no evidence to support the use of glucosamine and chondroitin sulfate to decrease or reverse the progression of arthritis. It works well for some and not at all for others. In addition, the U.S. Food and Drug Administration does not test dietary supplements before they are sold to consumers. These compounds may cause side effects if mixed with other supplements, and can interact with other medications.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your leg. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
Assistive devices. Using devices such as a cane, wearing shock-absorbing shoes, or wearing a brace or knee sleeve can be helpful.
Is there anything new that we can try? As a matter of fact there are some new treatment options available. Unfortunately we do not have a lot of research proving their long term benefits at this time. Platelet Rich Plasma (PRP) and Stem cells are two options available. Additionally, because they are so new, insurances will not cover the cost of these treatments. There has been a few new studies on PRP which demonstrate good results…and in some even better than corticosteroids or lubrications. In my experience in using PRP over the last few years we’ve had good results in knee arthritis pain relief. Again the worse the arthritis the more unpredictable the duration of pain relief.
Alternative therapies. Many alternative forms of therapy are unproven, but may be helpful to try, provided you find a qualified practitioner and keep your doctor informed of your decision. Alternative therapies to treat pain include the use of acupuncture, turmeric, CBD Oil, chiropractic care and magnetic pulse therapy.
Doc, how do I know when it’s time for a knee replacement?
This is probably the 2nd most common question I get, and a fantastic question at that! My response is “you will know when you’re ready”. When the symptoms from arthritis begin affecting your quality of life, your daily activities, your sleep, and you’ve tried several other nonsurgical options, it is probably time to have the discussion. For instance, if you’ve been taking an anti-inflammatory medicine, lost weight or been involved in therapy or an exercise regimen, had a steroid injection or two, and the pain still keeps you from enjoying daily activities we typically have “the talk”. Ultimately it is always YOUR decision and we will never try to talk you into surgery! Now you know everything I know about arthritis of the knee. I hope this bit is informative!
Thank you for trusting me with your care!! Dr. Colten Luedke